Exposing yourself to COVID-19
Posted by Richard on UTC 2020-03-24 15:33 Updated on UTC 2020-04-01
Update 26.03.2020 – Prof Dr Alexander Kekulé
Update 26.03.2020 – Nicholas Lewis: UK modelling errors
Update 27.03.2020 – Dr Deborah Birx: UK modelling errors
Update 01.04.2020 – Viral load
We always wondered why our family doctor, all those years ago in a small village in Germany, in many years of practice never seemed to fall ill.
Down the years epidemics came and went. At times his waiting room overflowed with the fevered, the sniffling and the perfectly healthy – hypochondria nests deep in the German soul. Usually one of our boys would be the cause of our presence, blood spattered, fresh from bike or skateboard, staunching the flow from head or knee with an old rag.
Asked on one occasion during a rather long stitching session how he managed to remain healthy despite this tide of human disease washing over him every day he replied that it was his belief that the nature of his job always brought him into early contact with the first sufferers in an epidemic.
According to him, that small, early 'infectious dose' gave his immune system time to kickstart before the pathogens arrived mob-handed. Even the hypochondriacs in his waiting room may have unwittingly immunised themselves against the real illness.
This concept of the 'minimal infectious dose' is well known to science, but is tricky to define – it is hardly possible to know exactly what quantity of pathogens have initially infected a sufferer.
Medical researchers, usually no shrinking violets, worry about the ethics of deliberately exposing humans to different doses of infections, even if they could somehow quantify the dose and systematise its delivery. The variability in the 'infectious response' of a host to any particular load would probably make the results of such experiments questionable anyway.
The concept has been useful in food hygiene, where one can count the number of pathogens present in a sample and produce a definition of some safe or acceptable level of such pathogens – after all, almost nothing in the real world is truly sterile, is it? But for diseases transmitted by contact or as aerosols between humans, how can you measure this?
Thus, although the minimal infectious dose is really a very important factor in epidemiology, it is only poorly understood and remains unquantified. Just one more thing that we do not know. Its importance is reflected in some aspects of the current outbreak of COVID-19 infections.
My saucy ship's a beauty
The first of these aspects concerns the interpretation of the results from the quarantine of the cruise ship Diamond Princess. The tale began on 19 January this year, when a certain person developed COVID-19 symptoms. The mean incubation period is around five days, so this person could have caught the infection somewhere between two and eight days before that.
Despite those symptoms, the person boarded the Diamond Princess in Yokohama the following day, 20 January and disembarked in Hong Kong on 25 January. This person was finally tested in Hong Kong on 1 February, nearly a week later, and tested positive.
During those five days, the infected person came in contact in some way with some of the 3,711 passengers and crew – and presumably left traces of the infection on every surface that he or she touched.
After the infected person had disembarked, the Diamond Princess continued the cruise with two stops in Vietnam, one stop in Taiwan and one stop in Japan before it finally reached Yokohama, where the ship was quarantined.
As already mentioned, the infected passenger disembarked on 25 January and the cruise ship returned to Yokohama on 3 February. Thus, following the five days the infected person was aboard, the passengers and crew experienced a further nine days of forced community.
On arrival in Yokohama the ship was immediately quarantined for 14 days and nearly all the passengers and crew were tested for COVID-19. In total, therefore, the passengers and crew on this floating Petri dish experienced 28 days of forced community.
Readers of the hysterical media would have expected the ship to be a floating coffin by the end of the quarantine – after all, more than three thousand people had been confined together in the closest proximity for around a month, whilst this terrible virus raged unchecked.
The results, though, are remarkable. Here they are as they stood on 25 February:
Summary of test positive COVID-19 cases by age group and symptom status onboard the Princess Cruises Ship.
| Age group |
Sympto- matic cases |
Asympto- matic cases |
Total | Crude asympto- matic ratio |
Persons aboard |
| 0-9 | 0 | 1 | 1 | 100% | 16 |
| 10- | 1 | 1 | 2 | 50.0% | 23 |
| 20- | 18 | 2 | 20 | 10.0% | 347 |
| 30- | 18 | 5 | 23 | 21.7% | 429 |
| 40- | 18 | 7 | 25 | 28.0% | 333 |
| 50- | 27 | 22 | 49 | 44.9% | 398 |
| 60- | 73 | 56 | 129 | 43.4% | 924 |
| 70- | 92 | 136 | 228 | 59.6% | 1015 |
| 80- | 27 | 25 | 52 | 48.1% | 215 |
| 90- | 2 | 0 | 2 | 0% | 11 |
| Totals | 276 | 257 | 531 | — | 3711 |
The 'crude asymptomatic ratio' is the proportion of asymptomatic cases among all the cases. This figure has to be treated with caution in cases where the cohort for that age is small (see the 50% figure for the 10-19 age group arising from two cases).
The table is adapted from Table 2 of Mizumoto and Chowell, Transmission potential of the novel coronavirus (COVID-19) onboard the Diamond Princess Cruises Ship, 2020, (25 February 2020)online.
According to a later paper (9 March 2020), which includes later results, by 20 February, 3,063 of the passengers and crew had been tested. Instead of the expected pile of steaming corpses, 634 persons had tested positive, that is, only 17% of those onboard. Of these positives, around half, 328, either showed no symptoms or developed symptoms after the test.
There was a total of seven deaths on the ship, all among those over 70 years-old. That is, out of the total of 3,711 persons, 0.89% died and out of the total of those who tested positive, 1.1% died. If this fatality ratio is applied to a population of 60 million we might expect a total of 113'177 people to die.
Of course, this kind of back of an envelope calculation is nonsensical. The fatality ratio from the Diamond Princess is difficult to apply to a standard population, since the average age of the passengers of the ship was 58 and the distribution skewed towards the elderly. We can, however, assume that they were all fit to travel and so only a few of them (if any) had serious underlying health conditions. In the general population this is of course not the case.
Let's sum up the remarkable features of these results.
- Despite confined life in this virus incubator, of the 3,063 people tested, 2,429 people tested negative – that is, 79% were unaffected by the disease.
- Of the 634 persons who tested positive, around half of these infected ones developed no symptoms. As the later paper shows, of the 3,711 passengers only 301 had any symptoms and only 7 died.
In the thirteen days between 5 February, when the quarantine was announced, and 18 February when the passengers were allowed to leave the ship, we do not know how passengers behaved in order to avoid infection. They had been ordered to stay in their cabins. Given that in the 15 days between the embarkation of the infected person and the imposition of the quarantine all the passengers and crew had circulated freely amongst themselves in bars, restaurants etc. the cabin isolation was certainly too little, too late.
In such confined circumstances, however, it is scarcely credible that around 80% of the people on the ship were able successfully to avoid infection by some form of 'social distancing' or contact hygiene. The crew would have became an engine of distribution of the virus whatever measures individual passengers took. We would suggest that everyone on the ship had a close encounter with this highly infectious virus in some form or other.
It is thus extremely difficult to explain why around 80% of the passengers and crew came through the experience unscathed. Unless for some unknown reason the situation on the Diamond Princess is a complete epidemiological aberration, it calls into question our modelling of the spread of the infection through normal life.
Put brutally: if 80% of the population will either not catch COVID-19 or hardly notice if they do, why are so many people being forced to suffer under lockdowns?
Flattening off
The media like to use the fright word 'exponential' when describing the spread of COVID-19. This is completely wrong: infections do not spread exponentially. They are not grains of rice added to a chess board, because infected people are not continually meeting new, uninfected people to whom they can pass on the disease.
Once the immediate family and the immediate work colleagues have been infected the person's role as a 'spreader' is more or less over – the torch is passed on, if at all, at a rate that is nowhere near exponential.
In a population, after a hesitant start, then a brisk inflation, the number of those infected flattens out into an asymptotic curve that approaches some peak value. The curve starts off as exponential but then turns into a logarithmic curve as it approaches the limiting asymptote.
The curve is known as the Gompertz Curve, in honour of its discoverer Dr Benjamin Gompertz (1779-1865) who first postulated it in 1825. Nearly two hundred years later it still hasn't passed into the minds of media commentators.
We can therefore assume that the epidemic on the floating Petri dish had largely run its course by the time the quarantine had ended – that is, even if the passengers and crew of the ship had been subjected to another month of quarantine, there would have been no marked increase in the number of cases of COVID-19.
It is arguable that one of the reasons for the surprisingly gentle passage of COVID-19 through the ship is the possibility that in this situation many of those on the ship received only a small infectious dose.
In other words, they were in the situation of the general practitioner mentioned at the beginning of this piece. We will never know, because this cohort was tested using a PCR test, which tests for the virus, not the antibodies it produces.
It is perfectly reasonable to imagine that the majority of those on the vessel were exposed to small doses of the virus by contact with surfaces or other passengers or as aerosols through the ventilation systems. By the time they were tested, their bodies had coped with the small number of invaders with a gentle, hardly noticeable immune reaction. This immune reaction would have been noticed had the cohort been tested for antibodies, not the virus, which, by this time had been obliterated.
Also, of course, not all viruses hit their mark, even if they find their way onto a human subject.
Medical personnel are exposed to far larger infectious doses from the ill and the dying and it seems that this may account for their relatively high mortality rate during this epidemic. Interestingly, during the quarantine period of the Diamond Princess, despite all the precautions that must have been taken, one quarantine officer, one nurse and one administrative officer tested positive for COVID-19.
Very interesting, the reader might say, but essentially speculation, not proof. That is true – never contradict your readers – but there is precious little proof available about anything when it comes to COVID-19. The complexity and variability of the underlying epidemiological data is impossible to render accurately with the simple single-number averages beloved by politicians, the media and their panjandrums.
But if the theory of the importance of the small infectious dose is correct, then the actions taken to slow down the spread of the infection among the general population may arguably be completely wrong-headed.
Using hand sanitizer, washing hands frequently, avoiding direct contact and applying social distancing may in fact be reducing the opportunity of the majority of the population to receive the sort of small infectious dose that will build up their immune systems.
If the government and its advisors were really serious about the much vaunted 'herd immunity', which is supposed to be going to save mankind from this plague, they might just try to let the herd get the little doses it needs to build up that immunity. After all, if you want immunity, you have first to catch the disease.
The only immunity that those sitting at home in enforced confinement will build up is to that much greater plague of modern civilisation, daytime television.
For a hard-headed academic statistician's analysis of the current epidemic go to the website of the estimable W.M. Briggs.
Update 26.03.2020
Our reader(s) will know that, as a change from our usual daydreams, we occasionally like to bring them the words of someone who knows what they are talking about.
On the present article's theme of the god of small doses, here is a brief excerpt of a response given by Prof Dr Alexander Kekulé, Professor of Medical Microbiology and Virology in Halle and Director of the Institute for Medical Microbiology there, to a caller on a radio programme about the COVID-19 epidemic.
Prof Kekulé's statement does not directly address the subject of minimal infectious dose, but illustrates well the probabalistic background to catching a viral disease.
The audio is the exchange in the original German. An English translation follows.
An excerpt of a radio broadcast by Prof Dr Alexander Kekulé. The programme was the eighth in a series, Kekulés Corona-Kompass, broadcast by MDR Mitteldeutscher Rundfunk on 24 March 2020.
[Schumann:] We have received a phone call from a listener, who despite Corona goes every morning to the bakers and therefore has the following question:
[Caller:] How long do the viruses survive on bread and rolls? And how long do the viruses survive on a newspaper?
[Kekulé:] Well, these questions are posed almost daily, I would say.
In essence, rough surfaces and biological surfaces are bad for the viruses – that is, on newspapers, cardboard and of course bread rolls and so on – on these they adhere for only a short while. Of course, an hour is possible, perhaps even two, plus or minus, but one should always consider the situation in terms of the quantity involved.
Even when the baker actually breathes out over the bread rolls in front of him and contaminates them with the aerosol he has produced, then the question still remains whether there are enough viruses to play a part in an infection.
That all has something to do with probabilities and for this reason I can only urgently appeal to people not to fall prey to hysteria about these smear infections (of the sort we know from films).
The situation is one in which as a rule one virus particle cannot trigger an infection. This arises mainly from the fact that a large majority of the viruses are incapable of causing an infection because they are so badly produced and have so many faults that the great majority of them that one can detect are not capable of causing an infection.
You can think of that as a production line which mainly turns out half-complete cars so that only something like every thousandth vehicle is capable of being driven. And therefore it is the case that a relatively large number of particles are required to trigger an infection– and then in addition they have to arrive at the right position on the host.
I would say that if one were to attempt to be 100% clean then you may as well stay at home and sit in a bath of 70% ethanol. People are unnecessarily paranoid about such things.
My recommendation is to concentrate on the infections caused by speaking and coughing, all those infections which are conveyed from the person generally standing in front of you – that constitutes the largest part of the transmission of the disease.
Update 26.03.2020
The independent researcher and statistics specialist Nicholas Lewis posted on his website yesterday an analysis of a paper produced by the COVID-19 Response Team from Imperial College London led by Prof Neil Ferguson.
It is fair to say that Ferguson's team has singled itself out in previous epidemics for the hysteria of its forecasting. Nevertheless, it is now the UK government's go-to source for epidemiological modelling on COVID-19.
Using the data from the Diamond Princess incident, Ferguson produced, as we would expect, an hysterical forecast of national death rates [Ferguson et al 2020].
In our article we swerved the issue of projected mortality rates on account of its complexity. But Nic knows what he is talking about and is highly qualified to venture into this territory. In addition, he is also one of those rarities, a scientist not dependent on generating panic in order to receive public grant money.
People interested in this topic should read his short paper (available on his site as a free PDF). As a taster, here is his table of case fatality estimates for the Diamond Princess:
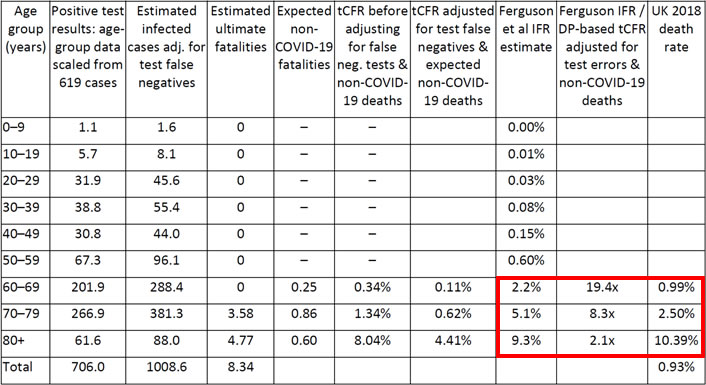
True Case Fatality Rates estimated from the latest Diamond Princess data compared with Infection Fatality Rates per Ferguson et al. 2019, used by the UK government.
Note: An all-causes tCFR of 0.34% (and hence 0.69 notional ultimate fatalities) is assumed for age-group 60-69 despite there being no actual fatalities in that age group (see text). Expected non-COVID-19 fatalities are based on UK 2018 death rates by age group applied to the DP positive test cases, scaled by the 45 day period over which COVID-19 deaths were recorded and divided by the same 0.96 factor used to scale up the 8 actual deaths. DP= Diamond Princess. The red box is from FoS.
Image: Nicholas Lewis, 'COVID-19: Updated data implies that UK modelling hugely overestimates the expected death rates from infection', 25 March 2020 [Click on the image to open a larger version in a new browser tab].
Update 27.03.2020
The wheels really have come off the COVID-19 modelling the Ferguson team has done. White House Coronavirus Task Force member Dr Deborah Birx delivered a stinging riposte to their work which should make them academically self-isolate for a few years at least.
I'm sure you have seen the recent report out of the UK about them adjusting completely their needs. This is really quite important. If you remember, that was the report that says there would be 500,000 deaths in the UK and 2.2 million deaths in the United States. They've adjusted that number in the UK to 20,000. Half a million to 20,000. We are looking at that in great detail to understand that adjustment.
I'm going to say something that is a little bit complicated but do it in a way we can understand it together. In the model, either you have to have a large group of people who a-asymptomatic, who never presented for any test to have the kind of numbers predicted. To get to 60 million people infected, you have to have a large group of a-symptomatics. We have not seen an attack rate over 1 in 1,000. So either we are measuring the iceberg and underneath it, are a large group of people. So we are working hard to get the antibody test and figure out who these people are and do they exist. Or we have the transmission completely wrong.
So these are the things we are looking at, because the predictions of the model don't match the reality on the ground in China, South Korea or Italy. We are five times the size of Italy. If we were Italy and did all those divisions, Italy should have close to 400,000 deaths. They are not close to achieving that.
Models are models. We are – there is enough data of the real experience with the coronavirus on the ground to really make these predictions much more sound. So when people start talking about 20% of a population getting infected, it's very scary, but we don't have data that matches that based on our experience.
And the situation about ventilators. We are reassured in meeting with our colleagues in New York that there are still I.C.U. Beds remaining and still significant – over 1,000 or 2,000 ventilators that have not been utilized.
Please, for the reassurance of people around the world, to wake up this morning and look at people talking about creating DNR situations, Do Not Resuscitate situations for patients, there is no situation in the United States right now that warrants that kind of discussion. You can be thinking about it in the hospital. Certainly, hospitals talk about this on a daily basis, but to say that to the American people and make the implication that when they need a hospital bed it's not going to be there or a ventilator, it's not going to be there, we don't have evidence of that.
It's our job collectively to assure the American people, it's our job to make sure that doesn't happen. You can see the cases are concentrated in highly urban areas and there are other parts of the states that have lots of ventilators and other parts of New York state that don't have any infected. We can meet the needs by being responsive.
There is no model right now – no reality on the ground where we can see that 60% to 70% of Americans are going to get infected in the next eight to 12 weeks. I want to be clear about that. We are adapting to the reality on the ground and looking at the models of how they can inform but learning from South Korea and Italy and from Spain and I know you will look up my numbers.
The only people who are over really one in a thousand cases are people that have very small populations like Monaco and Liechtenstein, so you will see a different number coming when your population is really tiny: one case can put you over one to a thousand or two to a thousand. Thank you.
Update 01.04.2020
The Lancet gets to grips with the concept of viral load: the more viruses in the host, the worse the disease is:
The mean viral load of severe cases was around 60 times higher than that of mild cases, suggesting that higher viral loads might be associated with severe clinical outcomes. We further stratified these data according to the day of disease onset at the time of sampling. The DCt values of severe cases remained significantly lower for the first 12 days after onset than those of corresponding mild cases (figure A). We also studied serial samples from 21 mild and ten severe cases (figure B). Mild cases were found to have an early viral clearance, with 90% of these patients repeatedly testing negative on RT-PCR by day 10 post-onset. By contrast, all severe cases still tested positive at or beyond day 10 post-onset. Overall, our data indicate that, similar to SARS in 2002–03, patients with severe COVID-19 tend to have a high viral load and a long virus-shedding period. This finding suggests that the viral load of SARS-CoV-2 might be a useful marker for assessing disease severity and prognosis.
Yang Liu et al. 'Viral dynamics in mild and severe cases of COVID-19', The Lancet, 19 March 2020. Our emphasis.
0 Comments UTC Loaded:
Input rules for comments: No HTML, no images. Comments can be nested to a depth of eight. Surround a long quotation with curly braces: {blockquote}. Well-formed URLs will be rendered as links automatically. Do not click on links unless you are confident that they are safe. You have been warned!